ASRA Pain Medicine Recommendations for Interventional Pain Procedures During Contrast Shortage
Click on the graphic below to download a PDF.
Contrast medium is frequently used to confirm accurate needle placement and injectate delivery and to exclude flow of off-target tissue in interventional pain procedures. In recent years, our world has been impacted by numerous supply-chain shortages, including medication shortages. Currently, iohexol is unavailable or in limited supply due to a shutdown of a production facility in Shanghai, China. Organizations and healthcare systems should provide guidance to clinicians during the shortage. Every attempt to conserve contrast for clinically appropriate interventions should be made. In the field of pain medicine, clinicians should consider minimizing iodinated contrast medium (ICM) use, using alternative image guidance (ultrasound [US]) when feasible, delaying interventions that are not clinically urgent, or using safer alternative contrast agents.
Should interventional pain procedures be delayed during the shortage of iohexol or other ICM?
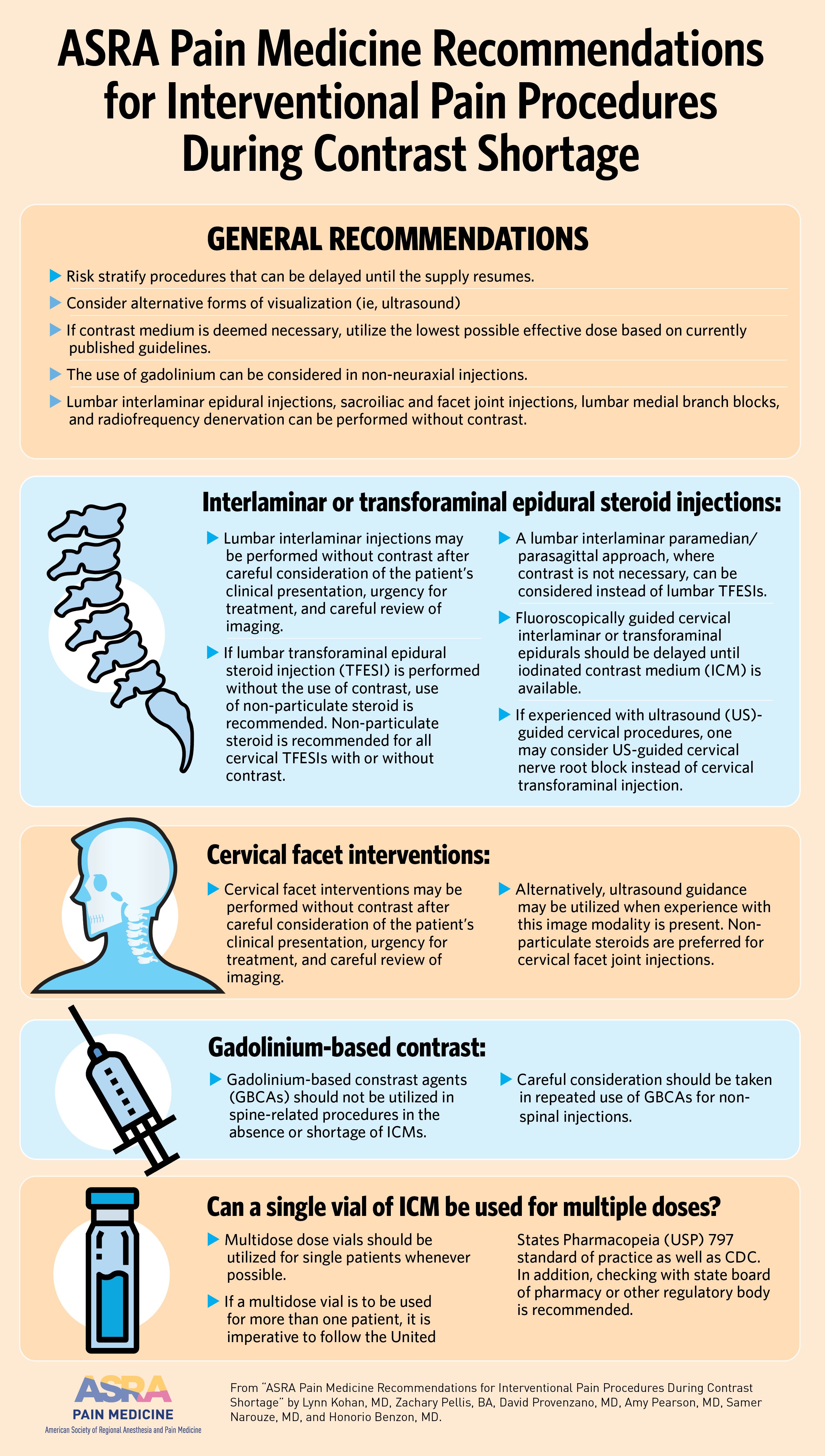
Attempts should be made to risk stratify procedures that can be delayed until the supply resumes. Patients with severe pain and functional impact should be prioritized, such as patients with suspected intrathecal drug delivery system malfunction who are in need of intrathecal catheter studies, particularly those with baclofen intrathecal delivery. Consideration should be given to alternative forms of visualization (ie, US) or the exclusion of ICM when nonessential for safety. The use of gadolinium can be considered in non-neuraxial injections.
Which interventional pain procedures can be performed safely without the use of iohexol or ICM?
A majority of fluoroscopically guided interventional pain procedures can be performed without the use of contrast agent. These include, but are not limited to, lumbar interlaminar epidural injections, sacroiliac and facet joint injections, lumbar medial branch blocks, and radiofrequency denervation. When a contrast agent is used, the minimum amount that does not reduce accuracy should be injected. Additionally, many procedures can utilize alternative image guidance such as US, including stellate ganglion blocks, joint injections, and deep soft tissue injections (eg, piriformis muscle). When performing these procedures under US, vascular structures can also be identified and avoided.
Can interlaminar or transforaminal epidural steroid injections (TFESIs) be performed without the use of contrast?
Given the current contrast shortage, clinicians must weigh risks versus benefits of performing these procedures without contrast. Lumbar interlaminar injections may be performed without contrast after careful consideration of the patient’s clinical presentation, urgency for treatment, and careful review of imaging.
Caution should be employed if considering lumbar TFESIs without the use of contrast given the increased risk of vascular compromise, in addition to risk of intradiscal spread. If lumbar TFESI is performed without the use of contrast, use of non-particulate steroid is recommended. Non-particulate steroid is recommended for all cervical TFESIs with or without contrast. In addition, a fluoroscopic depth view (lateral or contralateral oblique) is advised.
A lumbar interlaminar paramedian/parasagittal approach, where contrast is not necessary, can be considered instead of lumbar TFESIs in patients with unilateral radicular pain.
Fluoroscopically guided cervical interlaminar or transforaminal epidurals should be delayed until ICM contrast is available.
If experienced with US-guided cervical procedures, one may consider US-guided cervical nerve root block instead of cervical transforaminal injection.
Can cervical facet interventions be performed without the use of contrast?
Given the current contrast shortage, clinicians must weigh risks versus benefits of performing these procedures without contrast. Cervical facet interventions may be performed without contrast after careful consideration of the patient’s clinical presentation, urgency for treatment, and careful review of imaging.
If contrast medium is deemed necessary, utilize the lowest possible effective dose based on currently published guidelines.
Alternatively, US guidance may be used when experience with this image modality is present. Nonparticulate steroids are recommended in cervical facet joint injections.
Can alternatives to iodinated contrast such as gadolinium be used?
Gadolinium-based contrast agents (GBCAs) should not be used in spine-related procedures, such as interlaminar and TFESIs, in the absence or shortage of ICMs.
Careful consideration should be taken in repeated use of GBCAs for non-spinal injections.
Can a single vial of ICM be used for multiple doses?
Multidose dose vials should be used for single patients whenever possible.
If a multi-dose vial is to be used for more than one patient, it is imperative to follow the United States Pharmacopeia (USP) 797 standard of practice as well as Centers for Disease Control and Prevention guidance. In addition, checking with state boards of pharmacy or other regulatory bodies is recommended.
In summary, supply chain issues resulting in medication shortages are unlikely to resolve any time soon. Thus, we must be prepared to adapt while continuing to provide quality care to our patients.
Bibliography
American Hospital Association. FDA reports shortage of GE contrast media for CT imaging. Available at: https://www.aha.org/news/headline/2022-05-10-fda-reports-shortage-ge-contrast-media-ct-imaging. Accessed May 15, 2022.
Benzon HT, Maus TP, Kang HR, et al. The use of contrast agents in interventional pain procedures: a multispecialty and multisociety practice advisory on nephrogenic systemic fibrosis, gadolinium deposition in the brain, encephalopathy after unintentional intrathecal gadolinium injection, and hypersensitivity reactions. Anesth Analg 2021;133(2):535-52. https://doi.org/10.1213/ANE.0000000000005443
Centers for Disease Control and Prevention. Questions about multi-dose vials. Available at: https://www.cdc.gov/injectionsafety/providers/provider_faqs_multivials.html Accessed May 15, 2022.
Centers for Disease Control and Prevention. Questions about single-dose/single-use vials. 2019. Available at: https://www.cdc.gov/injectionsafety/providers/provider_faqs_singlevials.html Accessed May 15 2022.
Cohen SP, Bhaskar A, Bhatia A, et al. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Reg Anesth Pain Med 2020;45:424-7. http://dx.doi.org/10.1136/rapm-2019-101243
Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med 2022;47:3-59. http://dx.doi.org/10.1136/rapm-2021-103031
Rathmell JP, Benzon HT, Dreyfuss P, et al. Safeguards to prevent neurologic complications after epidural steroid injections: consensus opinions from a multidisciplinary working group and national organizations. Anesthesiology 2015;122(5):974-84. https://doi.org/10.1097/ALN.0000000000000614
United States Pharmacopeia. General chapter <797>: pharmaceutical compounding – sterile preparations. Available at: https://www.usp.org/compounding/general-chapter-797. Accessed May 20, 2022.
This practice advisory was first published May 23, 2022, and will be reviewed again in 2023.
Leave a commentOrder by
Newest on top Oldest on top