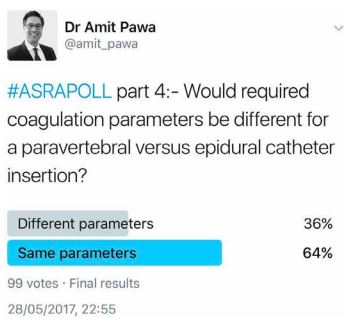
Problem-Based Learning Discussion (PBLD): Management of a Trauma Patient with Rib Fractures
CASE
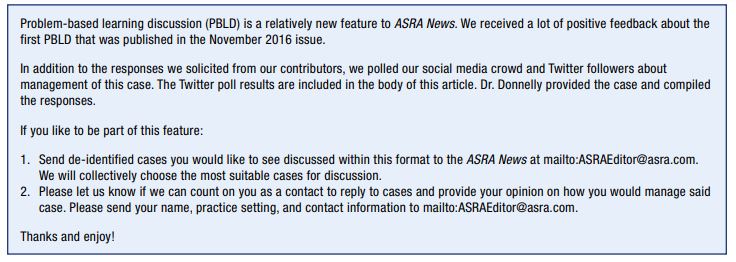
You are called by the trauma service to see a 76-year-old male who was recently admitted with bilateral rib fractures, T3 on the right and T4–T9 on the left (no other injuries) after falling off a ladder. He is currently on Bilevel Positive Airway Pressure (BiPAP) treatment. The trauma service requests a block for pain control. The only medical history that can be obtained from him is that he has diabetes and hypertension and had a nondebilitating stroke many years ago that left him with a slightly clumsy left foot and hand. The patient states he can’t remember all the medications he is currently taking but that they include insulin and metoprolol. His family is not currently available but should be at some point later today. He has not received care at your facility in the past. The trauma service would like a block to provide pain control in this patient because it is felt that pain is impairing adequate ventilation. The trauma service is hopeful that an epidural may help him avoid intubation.
1. How would you proceed at this point (epidural, paravertebral block/catheters, ketamine infusion, multimodal analgesia)?
Dr. Guha: Assuming that he (or someone else) is able to appropriately provide consent and the patient has no coagulopathies or other contraindications, I would offer an epidural. This would cover both the right- and left-sided rib fractures. Multimodal analgesia may be provided in addition to the epidural but is unlikely to offer the same degree of pain relief on its own that an epidural would.
Dr. Gilloon: Without a complete medical history, including complete medication list, and labs (ie, international normalized ratio [INR], platelet count), I would not proceed with an epidural or paravertebral. The patient has a history of stroke and could conceivably be on blood thinners. If he cannot verify a complete medication list, then his family, primary care provider, or pharmacy needs to be contacted. I appreciate the trauma team’s sense of urgency in wanting to prevent intubation; however, I would not risk performing an invasive procedure that could result in harming the patient. While trying to collect more information, I would initiate a ketamine infusion.
Dr. Jacob: I believe a midthoracic epidural would probably provide the most effective and durable pain relief option for his bilateral rib fractures, but I am hesitant to proceed without clarifying his medication list (specifically, whether he has been taking anticoagulant or antiplatelet medications) and laboratory studies. If his family is available later in the day to clarify his medical history and medications, then I would temporize his pain relief with multiple level intercostal blocks with bupivacaine or ropivacaine in addition to multimodal, non-opiate systemic analgesia.
Dr. Blake: This patient does not know which medications he is taking, and given his history of a stroke, I am concerned that he may be on an anticoagulant. I would not want to place an epidural or paravertebral blocks if the patient were in fact anticoagulated. I would want to check with the patient’s family and primary care provider first to confirm medications and history. I would also have an INR and platelets checked. Until further evaluation is possible, I would proceed with multimodal analgesia but try to avoid opioids. I would definitely consider a ketamine infusion as well.
Dr. Rustameyer: I would like to perform an epidural for this patient’s rib fractures.

2. What are the unique risks and benefits associated your choice of proposed therapy, and why did you choose it?
Dr. Guha: Epidural analgesia would provide superior pain control to opiates, ketamine infusion, or multimodal analgesia. In addition, it causes much less sedation and respiratory depression (it would cause none if the infusion consists only of local anesthetic and no opiates). Risks include nerve injury, bleeding, or infection. This patient has preexisting weakness in his left foot and hand, so further nerve injury could be potentially debilitating. If the patient’s medical history suggests a coagulopathy, I would check an INR and platelets to assess the risk of bleeding. However, the benefits would outweigh the risks in my mind.
Dr. Gilloon: A ketamine infusion is a noninvasive method to help control the patient’s pain. Unlike opioids, it will not suppress respiratory drive, which is particularly important in the setting of rib fractures. Although ketamine can have dissociative side effects, in my experience, patients typically tolerate it well on the floor
Dr. Jacob: A midthoracic epidural would afford the greatest ability to provide extended duration bilateral analgesia over multiple levels with a single catheter technique. My greatest concern would be placing a neuraxial catheter in a patient potentially taking antiplatelet or anticoagulant medications. I am specifically concerned about the risk for a neuraxial hematoma. He would also be at risk for hypotension due to the sympathectomy from the epidural block as well as the rare, but real, risk for neuraxial infection and neurologic injury.
Multiple injection intercostal blocks would also be effective but limited by a shorter duration of benefit even when using a longacting local anesthetic. Bleeding risk for intercostal block (even in an anticoagulated patient) should be minimal as long as the injection is performed away from the neuraxis in a compressible site (eg, midaxillary line). By performing multiple intercostal blocks, it would provide pain relief until the extended family arrives to obtain additional medical history and would also help clarify if his respiratory difficulty is indeed due to pain (secondary to the fractures) versus some other cause. If his respiratory status improves, then it provides stronger evidence that an extended duration block from a thoracic epidural would be beneficial.
Dr. Blake: I have chosen multimodal analgesia +/- ketamine infusion because I do not know the anticoagulation status of this patient and he has a history that puts him at increased likelihood of being on an anticoagulant. An epidural or paravertebral blocks could be contraindicated if he is in fact on certain anticoagulants. I believe that regional anesthesia may be superior for pain control, but multimodal therapy can provide some pain control without the risks posed by regional anesthesia in this situation. I have concerns about administering opioids to this patient and I would try to avoid them because they could further depress breathing or cause delirium/mental status changes in this elderly patient. Ketamine could contribute to pain control but may also potentially cause confusion, hallucinations, or other dissociative side effects.
Dr. Rustameyer: My biggest concern with an epidural is the coagulation status of a trauma patient with a history of a stroke. Therefore, I would want to check prothrombin time (PT)/INR on him prior to epidural placement. I would also need to get a more complete medication list prior to placement. The benefits to an epidural for bilateral rib fractures is that I can provide localized pain control with minimal cognitive interaction of the medications.
Thirty minutes into your consult, the labs return on this patient and reveal an INR of 1.4 and platelet count of 92K. All other values are normal, including liver function tests. The surgical team knows you have required a platelet count of 100K or higher for epidural placement and offers to do a platelet transfusion if you think it is necessary to proceed safely. They really want this block in and feel it will help him tremendously.
3. Describe your analgesic and management plan for this patient at this point along with justification for your decisions (if it is the same as in Q1 just say “same”).
Dr. Guha: I would ensure that the patient is not on any other anticoagulants or antiplatelet agents, including aspirin or NSAIDs. If not, I would still proceed with an epidural. If he is on other anticoagulant medications, I would recommend a nonregional technique, such as ketamine infusion and/or multimodal analgesia.
Dr. Gilloon: Same. They still have not verified the patient’s medication list. If the patient was on warfarin, his INR would need to be normal prior to proceeding with an epidural or paravertebral catheter. Even if the patient is not on warfarin, an elevated INR and low platelet count pose an increased risk of bleeding.
Dr. Jacob: I would not initiate neuraxial analgesia with an INR of 1.4, nor would I advise anyone to initiate treatment to lower an INR just to place an epidural. Therefore, I would proceed with multilevel intercostal block plus multimodal analgesia.
Dr. Blake: Same. I still do not know if the patient is taking any anticoagulants. The elevated INR could be the patient’s baseline, due to liver disease, or could indicate that the patient is on warfarin. The marginally low platelet count, as well as the somewhat elevated INR, puts the patient at some increased risk for bleeding, so if he is on an anticoagulant as well, I would definitely want to avoid an epidural or paravertebral block.
Dr. Rustameyer: With that platelet count, I would want to trend his platelets prior to placing a neuraxial catheter. Therefore, in this situation, I would keep him comfortable with multimodal analgesia and check another platelet count in 2 hours.
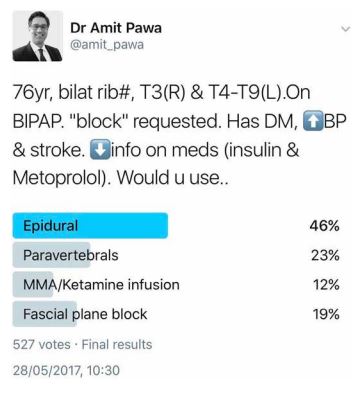
4. What institutional guidelines exist for placement of blocks in trauma patients (eg, medication history, coagulation parameters, spine clearance) for your practice? Are these guidelines standardized across your group and conveyed to surgical colleagues?
Dr. Guha: We do not commonly treat patients with rib fractures at our institution. We do not have specific guidelines in place for our institution regarding neuraxial techniques and anticoagulation. Instead, we rely on ASRA guidelines, which we communicate to our surgeons.
Dr. Gilloon: My group uses the ASRA guidelines from Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines, 3rd Edition to guide placement of blocks. The exact platelet count threshold varies by physician and clinical situation. We are a Level 3 trauma center and have a robust Acute Pain Service; however, we are rarely consulted for rib fracture analgesia management.
Dr. Jacob: Our institution does not have any formal policies or guidelines regarding placement of blocks in trauma patients. Cases are handled individually at the discretion of the attending anesthesiologist and in collaboration with surgery service.
Dr. Blake: At my institution, we try to follow the ASRA anticoagulation guidelines regarding medication history and coagulation parameters. In general, we want the spines to be cleared and the patient able to sit up for placement. There should not be fractures/issues in the immediate area of placement. If there are fractures/instability in other areas, a technique may still be performed as long as the patient is cleared for positioning, such as sitting or log rolling. Our guidelines are not completely standardized across our group. Some colleagues in my group are less conservative than others, and we all tend to use our own judgment at times. Our guidelines have been conveyed to our surgical colleagues on numerous occasions, but since we are an academic institution, we frequently have new residents that are not aware of these guidelines, and they are not always conveyed by faculty or senior level residents.
Dr. Rustameyer: None.
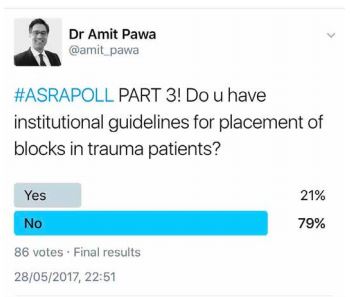
5. Would required coagulation parameters be different for a paravertebral versus epidural catheter insertion?
Dr. Guha: No, the required coagulation parameters would be the same for both regional techniques.
Dr. Gilloon: In my opinion, a paravertebral block is a deep plexus block, and the same ASRA guidelines employed for epidural catheters need to be applied.
Dr. Jacob: I would treat a paravertebral catheter identical to an epidural catheter.
Dr. Blake: At our institution, we generally treat paravertebrals as a neuraxial technique, so required coagulation parameters would be the same as epidural catheter insertion.
Dr. Rustameyer: I would have the same coagulation parameters for paravertebral and epidural catheter insertions. I treat them both as neuraxial blocks.
A family member arrives for this patient, and she provides some additional history: He is on aspirin 81 mg a day as a blood thinner, insulin, and metoprolol. She reports that he has no bleeding disorders. His labs are repeated and now his platelets are 101K, INR 1.2.
6. Would this information alter your previous analgesic plan and why?
Dr. Guha: Given that the repeat platelet count and INR indicate that the patient is less coagulopathic, I would proceed with an epidural catheter.
Dr. Gilloon: Yes, having a complete medication list that excluded blood thinners other than aspirin along with repeat labs showing platelets of 101 and an INR of 1.2 would make me comfortable performing an epidural. A properly placed epidural will provide better analgesia than a ketamine infusion. In my opinion, the potential epidural side effects (including hypotension, hematoma, abscess, etc) would be outweighed by the improved analgesia. If the rib fractures had been unilateral, I would have considered a paravertebral catheter due to the lower risk of hypotension. However, this patient would have required bilateral paravertebral catheters, which, in addition to requiring two procedures, would also have increased the amount of local anesthetic infusion.
Dr. Jacob: Yes. Assuming the patient and family consents to proceed, the normal INR level is acceptable to initiate neuraxial analgesia.
Dr. Blake: Potentially, depending on the timing between the two differing lab value sets and whether any treatments were given, such as platelets, fresh frozen plasma, or vitamin K. If no treatments have been given, I would opt to place an epidural catheter for pain control. The patient meets criteria per ASRA guidelines and an epidural would greatly benefit him in terms of pain control. It would hopefully reduce or avoid the need for opioids, which would be very beneficial for an elderly patient. I would choose an epidural over paravertebral catheters, because even though there is only one fractured rib on the right side and it is high thoracic, there is likely to be some bruising and pain on that side, and an epidural would provide more efficient and potentially effective bilateral pain relief. I would also utilize other forms of multimodal therapy in conjunction with the epidural.
Dr. Rustameyer: This information would encourage me to go ahead and place a thoracic epidural.
7. Where would you place an epidural or paravertebral catheter(s)? What would your infusion be and what side effects might you predict? Are there differences in how these are dosed/test dosed/placed versus thoracic catheters for pre-surgical patients?
Dr. Guha: I would place the epidural at T6 to maximize the chance that local anesthetic would spread cephalad and caudad enough to cover all the rib fractures. My infusion would consist of bupivacaine 0.125% + hydromorphone 10 mcg/mL. (If the patient appeared somnolent or there were contraindications to opioids, I would run only bupivacaine 0.125%). I would run the infusion at 6 mL/hr with a patient-controlled bolus of 4 mL to be given every 30 minutes as needed. The placement, dosing, and test dosing would be the same as for presurgical patients. One difference is that this patient is already experiencing pain and may require a greater level of preprocedure sedation and/or pain control so that he is comfortable enough to sit up for epidural placement.
Dr. Gilloon: I would place the epidural at T6 centered among the fractures. At my institution, we use ropivacaine exclusively, with or without fentanyl. I would start with 0.1% ropivacaine with fentanyl 2 mcg/mL at 6 mL per hour with patient-controlled epidural analgesia of 4 mL every 30 minutes. If the analgesia band proved too narrow, I would titrate the rate up to 10 mL. If the patient’s blood pressure proved stable and he had persistent pain, I would consider increasing the concentration of ropivacaine from 0.1% to either 0.15% or 0.2%. Side effects from the epidural placement could include hypotension, pruritus, nausea, sedation, and, less commonly, local anesthetic systemic toxicity. If the patient were exhibiting nausea, pruritus, or sedation, I would remove the opioid from the epidural.
Placement of an epidural in the setting of rib fractures compared to a presurgical patient can be more challenging due to the patient’s diminished ability to cooperate with positioning secondary to pain.
Dr. Jacob: I would plan to place a thoracic epidural in the T5–6 or T6–7 space, centrally located to allow for adequate cranial spread to T3 and caudal spread to T9. After placement, I would test with a standard 3 mL 1.5% lidocaine + 1:200k epinephrine solution, followed by a 5 mL loading dose of 0.25% bupivacaine. Once loaded, I would initiate a continuous infusion 6 mL/hr of 0.075% bupivacaine mixed with hydromorphone 5 mcg/mL. The main side effect I anticipate would be hypotension. I would initiate, dose, and treat this catheter as I would for any patient having an equivalent level chest surgery.
Dr. Blake: I would place an epidural at level T6/7. This would place it in the middle of the left-sided rib fractures to hopefully get spread that will cover all of the fractures for maximal pain relief. It would be difficult to cover the T3 fracture on the right side; this is another reason multimodal therapy as an adjunct would be beneficial. I would start an infusion of 0.1% ropivacaine with a rate of 5 mL/hr. I would not add opioids to the infusion in this elderly patient to avoid any mental status changes, confusion, etc.
In presurgical patients, there are typically no limitations in positioning—most patients are able to maintain a sitting position for placement. In trauma epidural patients, there are frequently positioning limitations where patients will be lateral decubitus and may or may not be able to curl into an optimal position.
Infusions in presurgical patients at my institution are typically initiated with 0.1% ropivacaine and 10 mcg/mL hydromorphone at a rate of 6 mL/hr. In trauma epidural patients, we often use a local anesthetic solution without opioid or put the opioid on a separate epidural pump. This allows discontinuation of the opioid if the patient becomes confused or has mental status changes, often in elderly patients. It also allows discontinuation of the local anesthetic infusion if the patient becomes hypotensive or has cardiovascular instability. I generally treat the test dose similarly between these two groups of patients—typically 3 mL of 1.5% lidocaine with epinephrine. If the trauma epidural patient is stable after the initial test dose, from a cardiovascular standpoint, I will often administer the other 2 mL of test dose that comes in the epidural kit.
Dr. Rustameyer: I would place this epidural at T6–7. I’d start the infusion at 4 mL/hr and increase it 1 mL/hr until adequate coverage was achieved. The side effects I’d expect would be bradycardia and hypotension if the epidural solution affected the cardiac accelerator fibers. This is why I’d start with a low infusion and increase it slowly.
You decide to place a T6/7 epidural. The patient feels his pain is much better controlled just 2 hours after placement, and he has weaned off BiPAP to nasal cannula 4L. The team provides deep vein thrombosis (DVT) prophylaxis in the form of once daily low molecular weight heparin (LMWH). His aspirin is stopped, and he continues his other home pain medications.
Three days later, the patient is doing well on oral meds and after the epidural has been shut off for 3 hours. He had his LMWH held this morning but, unfortunately, a medication error occurred on your patient and he received one 75 mg dose of clopidogrel yesterday morning. The team is hoping you can remove the epidural so they can send him home tomorrow.
8. How will you proceed with epidural management/possible discontinuation for this patient?
Dr. Guha: ASRA does not make any specific requirements regarding time interval to wait from last dose of clopidogrel until removal of epidural catheter. I would first ensure that the previous coagulopathy and thrombocytopenia had been corrected and that the patient was not on any other anticoagulant or antiplatelet agents. I would then wait five half-lives from the time of the last clopidogrel dose and then remove the epidural catheter. LMWH administered once daily for DVT prophylaxis must be held for 12 hours prior to catheter removal and not restarted until 4 hours later, as per ASRA guidelines. I would monitor the patient for another 24 hours in the hospital after catheter removal with frequent neurological assessments to ensure he is not developing signs of an epidural hematoma.
Dr. Gilloon: The drug error is unfortunate and complicates the epidural management. The ASRA guidelines recommend holding clopidogrel for 7 days prior to epidural placement and withholding clopidogrel while the catheter is in place. However, they do not give guidance regarding a single dose of clopidogrel that is administered in a patient with an epidural catheter. I typically apply the same guidelines for epidural placement to epidural removal. In my opinion, it is not practical to leave the epidural in place for 7 additional days due to this single dose of clopidogrel. I would discuss the medication error with the patient and recommend withholding additional doses of LMWH. I would wait 5 half-lives of clopidogrel (30 hours) and remove the catheter. I would educate the patient and family on signs of epidural hematoma, including back pain, numbness, and paralysis. If the patient understood and could self-monitor or had reliable caregivers, I would have the patient discharged a few hours after the catheter was removed.
Dr. Jacob: I would remove the catheter, order every-4-hour neuro checks for 24 hours to assess lower extremity motor and sensory function, and request LMWH be held until the next morning.
Dr. Blake: After a single 75-mg oral dose, the half-life of clopidogrel is approximately 6 hours. It takes 3 to 7 days of clopidogrel dosing to reach a steady state of platelet inhibition. I would make sure that the team does not give any further clopidogrel or LMWH. I would have a discussion with the team, patient, and patient’s family about the risks of bleeding and hematoma formation with removing the epidural. It is not very practical to keep the patient in the hospital for 7 days from his single dose of clopidogrel, for which the half-life is 6 hours. After a thorough discussion of risks and benefits, I would likely remove the epidural the following morning (2 days after his clopidogrel dose and 24 hours after his last dose of LMWH). I would strongly consider keeping him in the hospital that day and possibly one more night for neurologic monitoring. When the patient does discharge home, I would make sure myself or someone on my team follows up with him at home via phone.
Dr. Rustameyer: If possible, I would assess platelet function. Giving a platelet transfusion would be something else I’d consider. If I was not able to assess platelet function, I wouldn’t be willing to pull the epidural catheter for approximately 48 to 72 hours.
Leave a commentOrder by
Newest on top Oldest on top